Senator sounds alarm on healthcare impacts from federal spending bill
Cortez Masto warns of ripple effects beyond Medicaid recipients in Southern Nevada
Nevada’s senior senator is raising red flags about proposed federal legislation that could fundamentally alter healthcare access across the Silver State, warning that impacts would extend far beyond those currently relying on government assistance programs.
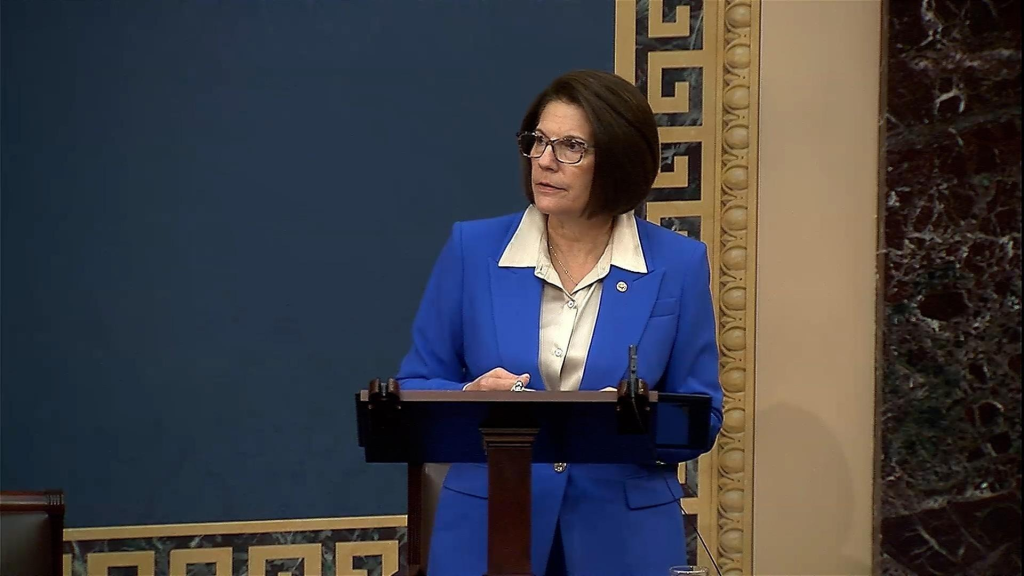
U.S. Senator Catherine Cortez Masto has emerged as a vocal critic of what Republicans have dubbed the “one big beautiful bill,” arguing that the sweeping legislation threatens to destabilize Nevada’s entire healthcare ecosystem. Her warnings come as the state’s healthcare providers brace for potential funding cuts that could affect hundreds of thousands of residents.
Beyond Medicaid: Private insurance holders face consequences
While much attention has focused on the bill’s impact on Medicaid recipients, Cortez Masto emphasizes that privately insured Nevadans won’t escape unscathed. The senator predicts a domino effect that could touch virtually every aspect of healthcare delivery in the state.
“People that don’t rely on Medicaid, and just have regular insurance or have—are able to get insurance through their work, they’re going to see their prices go up,” Cortez Masto explained during recent discussions about the legislation. She warned that accessing medical care could become increasingly difficult, with longer wait times and reduced availability becoming the new normal.
The mechanism behind these widespread impacts lies in how healthcare systems operate. When government reimbursements decline, providers must compensate for losses elsewhere, typically by increasing costs for privately insured patients or reducing services altogether.
Rural hospitals face existential threat
Perhaps nowhere would the legislation’s impact be felt more acutely than in Nevada’s rural communities, where hospitals already operate on razor-thin margins. The proposed Medicaid reductions could prove catastrophic for these facilities, many of which rely heavily on government reimbursements to keep their doors open.
Cortez Masto expressed particular concern about the cascade effect of rural hospital closures. Patients from outlying areas would be forced to seek care in urban centers, potentially overwhelming Las Vegas and Reno hospitals that are already operating near capacity. This influx could strain emergency departments and create longer wait times for all patients, regardless of insurance status.
The geographic challenges facing rural Nevadans cannot be overstated. In some parts of the state, residents already drive hours to reach the nearest medical facility. Hospital closures would transform difficult journeys into impossible ones, potentially leaving entire communities without reasonable access to emergency care.
Numbers paint stark picture
According to various estimates, the legislation could result in approximately 114,000 Nevadans losing their health coverage. This figure includes an estimated 70,000 who would be removed from Medicaid rolls and another 40,000 who could lose coverage under the Affordable Care Act.
The Congressional Budget Office projects that the bill would cut Medicaid funding by $930 billion over the next decade. For a state like Nevada, which has worked to expand healthcare access in recent years, such reductions would represent a significant reversal of progress.
Healthcare advocates note that among Nevada’s Medicaid recipients, 39% are children and 15% have chronic conditions requiring ongoing medical care. These vulnerable populations would face the most immediate and severe consequences from coverage losses.
Political divide emerges
The legislation has created a clear partisan divide within Nevada’s congressional delegation. Both Democratic senators—Cortez Masto and Jacky Rosen—voted against the measure, citing concerns about its impact on working families and healthcare access. Meanwhile, the state’s House delegation split along party lines, reflecting the broader national debate over healthcare policy and government spending.
Republican supporters of the bill have included provisions they argue would help rural hospitals weather the funding changes. However, critics question whether these measures would be sufficient to offset the broader cuts to Medicaid reimbursements.
Healthcare providers prepare for uncertainty
Across Southern Nevada, healthcare administrators are already conducting assessments to determine how the proposed cuts might affect their operations. Some facilities are exploring contingency plans that could include staff reductions, service eliminations, or in worst-case scenarios, closures.
Northern Nevada HOPES, a community health center serving thousands of patients annually, exemplifies the concerns facing providers. With approximately 40% of their patients relying on Medicaid, significant funding reductions could force difficult decisions about which services to maintain and which locations to keep open.
University Medical Center and other major hospitals are similarly evaluating their exposure to Medicaid cuts, knowing that any reduction in government reimbursements would need to be offset through other revenue sources or operational changes.
Broader economic implications
The healthcare sector represents a significant portion of Nevada’s economy, providing thousands of jobs and billions in economic activity. Healthcare advocates warn that the proposed cuts could trigger job losses extending beyond direct medical positions to support staff, administrators, and ancillary services.
Moreover, the ripple effects could impact Nevada’s ability to attract and retain businesses. Companies considering relocation often evaluate the quality and accessibility of local healthcare when making decisions. A degraded healthcare system could make Nevada less competitive in economic development efforts.
Looking ahead
As the legislation moves through the federal process, Nevada’s healthcare community remains on edge. The state’s unique demographics—including a large service industry workforce often lacking comprehensive insurance and a rapidly growing senior population—make it particularly vulnerable to healthcare disruptions.
For Southern Nevada specifically, the region’s explosive growth has already strained healthcare infrastructure. Additional pressure from funding cuts and potential facility closures could exacerbate existing challenges in meeting the population’s medical needs.
The debate over this legislation represents more than a policy disagreement; it’s a fundamental question about healthcare access in Nevada. As federal lawmakers continue their deliberations, the state’s residents, healthcare providers, and political leaders watch anxiously, knowing that the outcome could reshape medical care delivery for years to come.
Whether the final version of the bill includes modifications to address these concerns remains to be seen. What’s clear is that Nevada’s healthcare system stands at a crossroads, with decisions made in Washington poised to reverberate through every hospital, clinic, and medical office across the Silver State.
Category: State News, Politics
Subcategory: Healthcare
Date: 07/11/2025




